Op-Ed: America's Health Care Depends on Women – Verywell Health
Meghan Fitzgerald, RN, MPH, DrPH, is an adjunct associate professor with the Columbia University Mailman School of Public Health and a private equity investor.
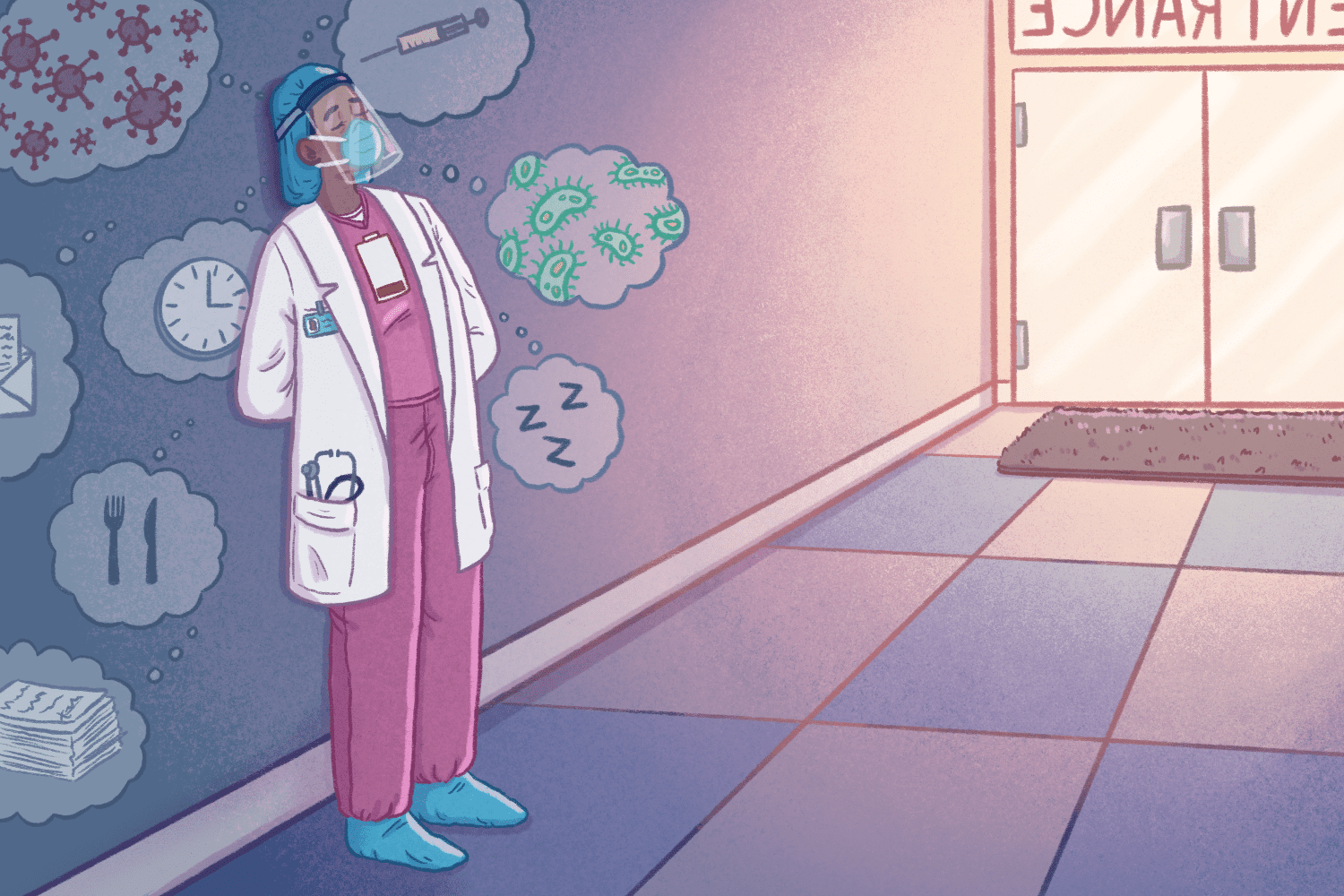
Verywell / Brianna Gilmartin
Meghan Fitzgerald, RN, MPH, DrPH, is an adjunct associate professor with the Columbia University Mailman School of Public Health and a private equity investor. She has decades of experience working in the healthcare field, ranging from frontline patient care to advising prominent healthcare firms. Here, she explains why the American healthcare system won't bounce back without making deliberate improvements for women.
Despite the ongoing challenges with COVID-19, in less than two years’ time, the United States has nearly returned to full employment with an unemployment rate of 3.9%, compared to 14.8% in April of 2020. It is a much speedier recovery than what was seen after the 2007-2009 global financial crisis. However, this success story is overlooking the lack of women currently in the workplace, whose labor force participation has hit a 33-year low. Out of all the COVID job losses, women compromised 60%.
This dynamic gets serious fast when we talk about our fragile healthcare system, which is under assault from Omicron surges, pent-up demand, inconsistent policies, and catastrophic losses of labor. Health care job growth for women in 2021 stagnated and then turned negative. Women hold 76% of all healthcare positions (89% of home health aides are women, 91% of nurses are women) so it’s fair to say our U.S. health care system recovery depends on a viable women-led workforce.
In health care, staffing shortages have hit the hardest in areas led by women, including outpatient nursing care facilities and home care.
Our healthcare system cannot call in sick.
To craft a viable plan, we must address three major challenges for working women in health care.
Women in health care are more likely to serve as caregivers for their family members—whether children or adults—than their male counterparts.
Despite 73% of Americans supporting paid family leave, the Build Back Better economic recovery package—which includes caregiving relief—is still being debated. Meanwhile, pandemic-era programs to help families have expired, like in the Families First Coronavirus Response Act and child tax credit payments.
While partisan politics continue to kick the can down the road, healthcare employers and employees are forced to get "creative." This means extended shifts, using overtime, and relying on staffing agencies—none of which are sustainable for workers, patients, or a system equipped to withstand a future crisis.
By nature, much healthcare work must be in-person. For example, 97% of patients receiving home care require assistance bathing. Still, the use of remote patient monitoring can triage scarce resources while telehealth can scale an employee’s value. Employers should seek inspiration from innovative peers around flexible shifts, respite care, job shares and rotations. The priority is to improve employee mental health, function, and retention. All frontline workers should be provided an opportunity to receive mental health check-ins and resources without fear or stigma.
Over the next decade, healthcare support roles are projected to experience the fastest job growth. However, research has shown four-year degrees are out of reach for many, with 44% of women citing affordability and 36% citing child care as obstacles. Healthcare can’t wait. The government must fund trade, vocational, and certificate degrees to onboard a new pipeline of workers beginning in high school.
The pandemic has mobilized a generation of youth who desire to work in health care, but need an on-ramp into affordable degrees to do so. Those who start with trade degrees have an opportunity to gain experience before climbing the health care ladder with subsequent degrees and training.
Pandemics throughout history are remembered by their impacts, not just the severity of illness. Disruptions during pandemics frequently gave way to economic opportunity once the pandemic subsided. Yet history finds periods of sociopolitical strife due to delayed and uneven economic recoveries. Given that 76% of full time health care jobs are held by women and female labor force participation took a big hit during the pandemic, we need to focus our efforts on remediating and reversing these issues.
Sign up for our Health Tip of the Day newsletter, and receive daily tips that will help you live your healthiest life.
Thank you, {{form.email}}, for signing up.
There was an error. Please try again.
U.S. Bureau of Labor Statistics. Labor Force Statistics from the Current Population Survey.
Congressional Research Service. Unemployment Rates During the COVID-19
Pandemic.
National Women's Law Center. A year of strength and loss: the pandemic, the economy, and the value of women's work. March 2021.
Smiley RA, Ruttinger C, Oliveira CM, et al. The 2020 national nursing workforce survey. Journal of Nursing Regulation. 2021;12(1):S1-S96. doi:10.1016/S2155-8256(21)00027-2
Thank you, {{form.email}}, for signing up.
There was an error. Please try again.